Osteoporosis can cause brittle, thinning bones as we age, but bone mass measurements, also known as bone density tests, can determine if you are at risk of fractures. Bone density tests can identify a decrease in bone density before you suffer a break, confirm a diagnosis of osteoporosis, and monitor treatment of osteoporosis, but should your doctor recommend it for you?
Doctors may order a bone density test if a patient has experienced:
- Decreased height
- Fractured bone
- Long-term use of steroid medications, such as prednisone, which can interfere with the process of bone-building
- Received a transplant of an organ or bone marrow
- Drop in hormone levels (due to some cancer treatments or menopause)
What to Expect
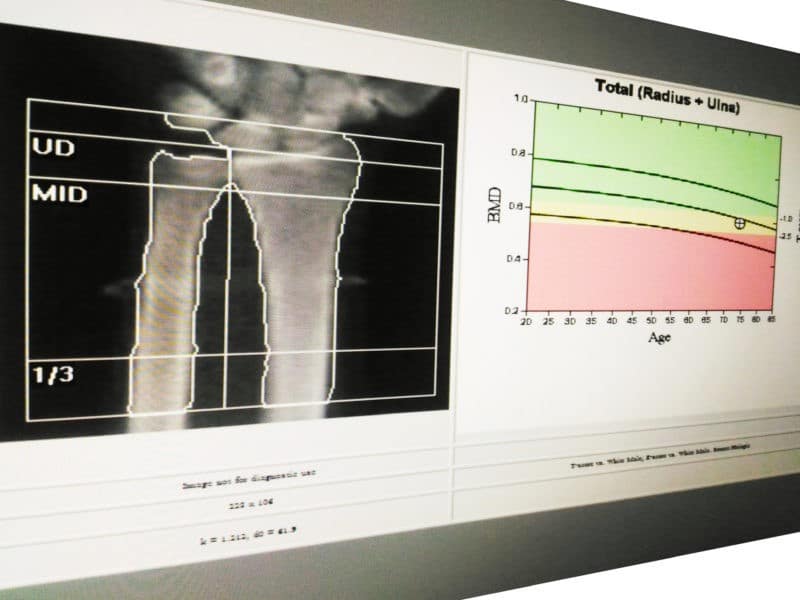
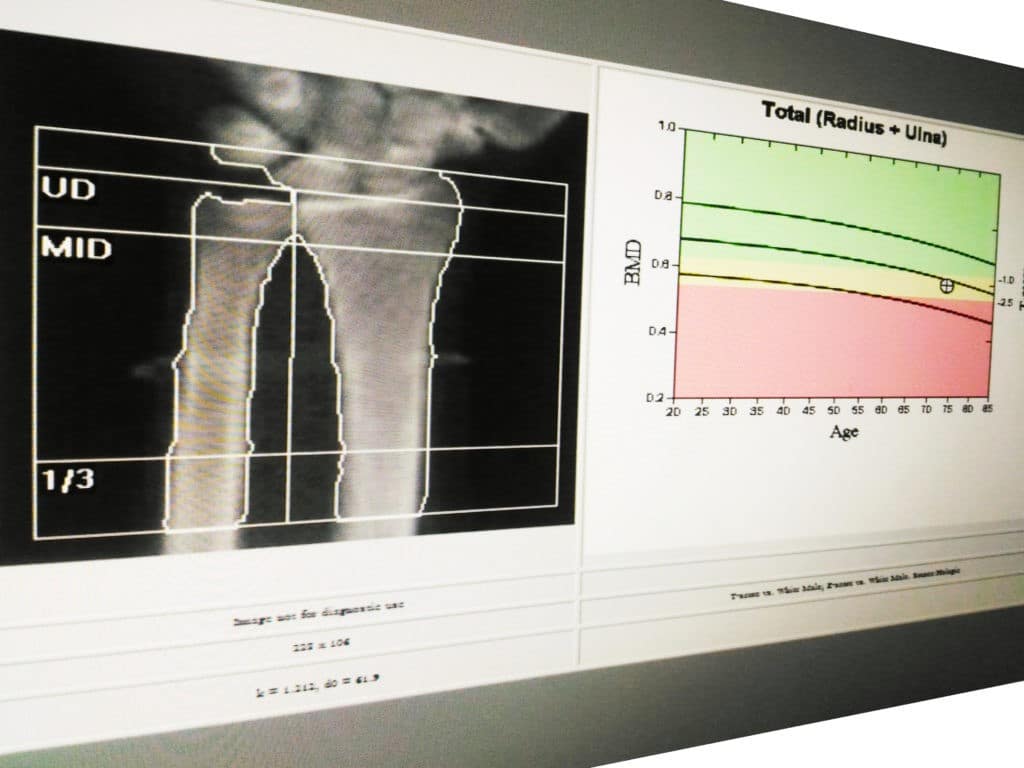
Bone density tests are painless and don’t require much preparation. Aside from avoiding calcium supplements 24 hours in advance, you should wear loose, comfortable clothing. Several bone density tests use ultrasound, urine tests, and X-rays or some form of radiation, such as:
- DXA (Dual-energy X-ray Absorptiometry)
- QCT (Quantitative Computed Tomography)
- RGA (Radiographic Absorptiometry)
How Medicare Can Help
Medicare Part B (Medical Insurance) covers a bone density test once every 24 months for individuals who meet the following criteria:
- A woman at risk for osteoporosis and is estrogen deficient
- A person whose X-rays show possible osteoporosis, osteopenia, or vertebral fractures
- A person taking prednisone or steroid-type medications, or is planning to take them
- A person diagnosed with hyperparathyroidism
- A person being monitored during osteoporosis drug therapy
The test may be ordered more often if your physician deems it medically necessary. If you have Original Medicare, you will pay nothing for this test as long as your doctor accepts assignment. If you are enrolled in a Medicare Advantage, you will have at least the same coverage as Original Medicare, but you may have additional benefits.